The Delta Variant (‘Delta’) of COVID-19 was designated a Variant of Concern by the World Health Organisation in May this year. Since an outbreak in India that peaked at around 400,000 cases per day (4x the size of India’s initial COVID-19 wave), Delta has been found in 130 countries including the UK, the US and now Australia and New Zealand. It has proved more difficult to contain and the World Health Organisation estimate it is twice as transmissible as the ancestral COVID-19 virus. Importantly, vaccines are proving highly effective in preventing severe illness. We have the capability to live with the Delta variant and move forward, whilst noting significant inequality in vaccine availability exists globally.
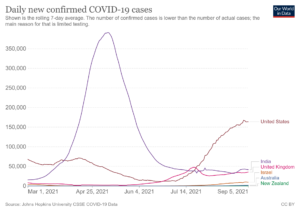 As you will note from the countries in the chart above, Delta has not spared countries with the highest vaccination rates. For example, Israel, one of the global leaders in its vaccination rollout, has fully vaccinated at around 62% of its total population and is now in the midst of a serious Delta wave. We are seeing a similar story in both the United Kingdom and the United States with vaccination rates of around 64% and 52% respectively. Although it is important to note that these countries are no longer using lockdowns to prevent the spread of the disease. Regardless, it is clear that the rates of vaccination we are seeing in these countries are not high enough to prevent a wave of reported COVID cases.
As you will note from the countries in the chart above, Delta has not spared countries with the highest vaccination rates. For example, Israel, one of the global leaders in its vaccination rollout, has fully vaccinated at around 62% of its total population and is now in the midst of a serious Delta wave. We are seeing a similar story in both the United Kingdom and the United States with vaccination rates of around 64% and 52% respectively. Although it is important to note that these countries are no longer using lockdowns to prevent the spread of the disease. Regardless, it is clear that the rates of vaccination we are seeing in these countries are not high enough to prevent a wave of reported COVID cases.
However, all is not lost. Vaccines are fulfilling their most important job in the fight against Delta – protecting people from becoming seriously ill. Data out of the United Kingdom points to vaccine efficacy at preventing severe cases and hospitalisations with the Delta variant is high, in the realm of 90% (albeit slightly reduced when compared to efficacy against the Alpha variant).1 This means that if you are fully vaccinated and contract the Delta variant, you are significantly less likely to end up severely unwell and in hospital compared to an unvaccinated person. Aside from the obvious health benefits, high vaccination rates markedly reduce the risk that hospitals will be overrun, which is one of the key metrics for allowing economies to remain fully functional.
The global vaccination effort is well underway but inequality exists and the challenge is increased by waning vaccine efficacy over time. Individuals vaccinated earlier in the pandemic now have a lower level of protection compared to those vaccinated later. This has led to countries commencing booster programs, offering a third vaccine dose to those who have already received two doses. In August, Israel opened this up to all individuals aged 12 years and older, provided at least five months have passed since their second dose. The United States has announced plans to roll out boosters from September, joining other developed countries including Canada, France and Germany which have also planned booster programs. Unfortunately the distribution of vaccines is not equitable, around 39% of the world’s population have now received at least one dose of a COVID-19 vaccine, compared to only around 1.6% of people in low-income countries. The World Health Organization has appealed to wealthy nations to defer distributing booster shots, to give more people in developing countries a first dose of the vaccine.
COVID causes disruption in many ways, the most significant being when leaders need to use lockdowns to protect people and prevent hospitals being overrun. As vaccines are rolled out globally, the proportion of populations fully vaccinated and thus protected against severe disease is increasing rapidly. This means that even if it doesn’t feel like it right now, it is starting to look like there is light at the end of the tunnel.
In the United Sates, case numbers look to have peaked in a number of the early Delta outbreak states and the pace at which case numbers and hospitalisations are rising has slowed, indicating they are moving closer to a nationwide peak. The pace of vaccination in Australia has increased dramatically and based on current vaccination rates, around 70% of the eligible population will be vaccinated by the end of October. In New Zealand, Dr Ashley Bloomfield has pointed to a around 90% probability the reproductive number (R0) of the virus has fallen below one, and we are seeing case numbers start to fall. Most importantly, available vaccines provide good protection against severe illness from known COVID-19 strains. We place a low probability on a variant emerging that evades vaccine protection, though it remains a watch item. The World Health Organisation has highlighted that the risk of variants emerging that are more potent than Delta, increases if the virus is left to spread rapidly in countries with low vaccination rates.
Milford continues to monitor and adjust our portfolios, and remain optimistic that over time we will continue to adapt to COVID – and its variants.


